Understanding Hairy Cell Leukemia: Diagnosis, Treatment and Beyond
Here you will find evidence-based information about hairy cell leukemia. Scroll this page or use the navigation links to read about how HCL is Diagnosed and common Symptoms>>, the types of Treatment (standard and new)>>, some Complications that you might experience>>, what it means to have Refractory or Relapsed HCL>>, and why Variant HCL>> differs from the classic form of the disease. The content on this page has been reviewed by medical experts at HCL Centers of Excellence.
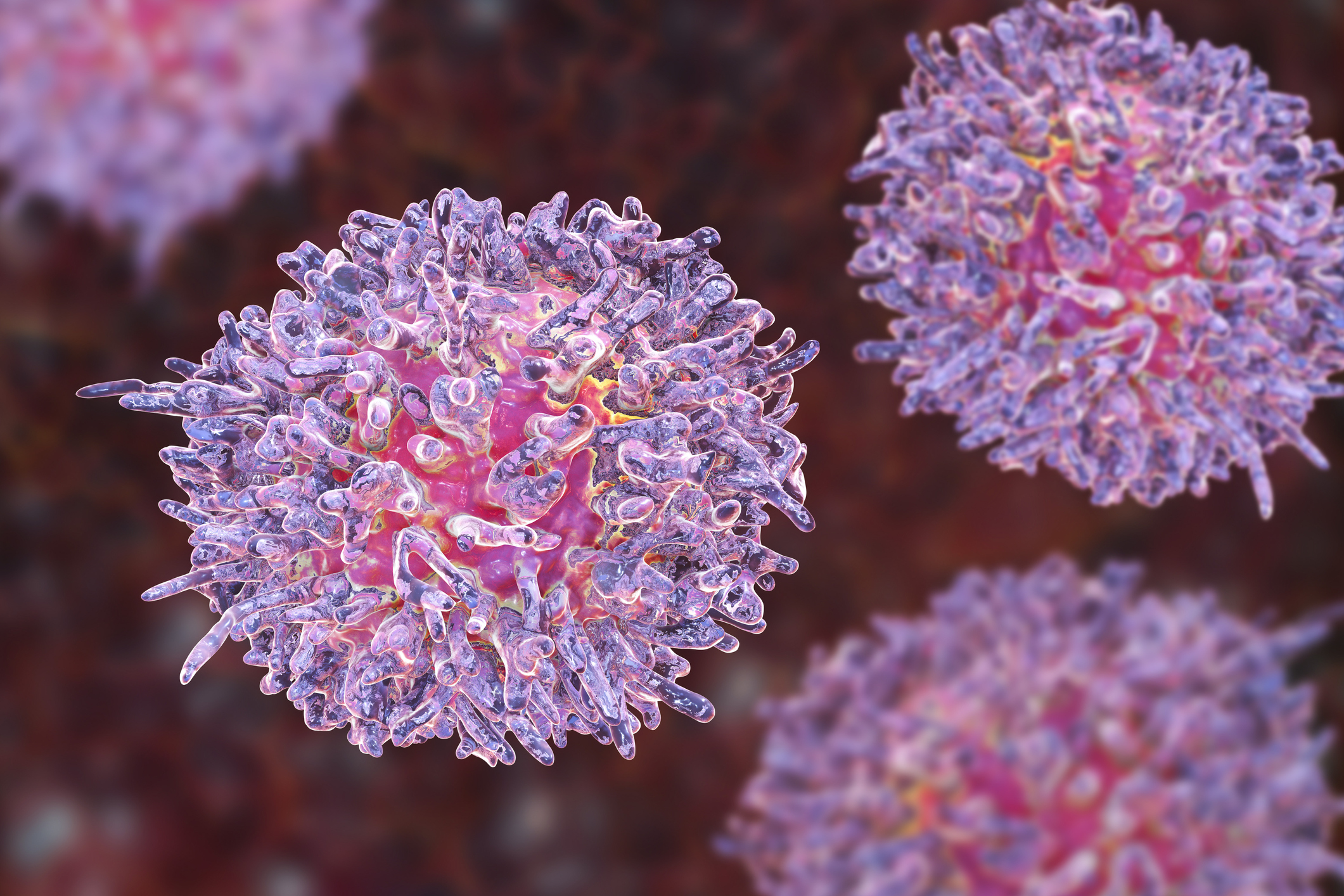
What is Hairy Cell Leukemia?
Hairy cell leukemia is a chronic and rare form of adult leukemia. It is estimated that approximately 2% of adult patients with leukemia have this form of disease. While the cause of this malignancy is not known, the origin of the malignant cell is thought to develop from the memory B cell compartment. These malignant cells infiltrate the bone marrow, the spleen, and the liver from the time of diagnosis. While lymph nodes in the abdomen may be involved, lymph nodes are rarely enlarged on physical examination.
Hairy cell leukemia is usually gradual in onset. Patients present with fatigue, increased susceptibility to infection, and enlargement of the spleen. The malignant hairy cells in the bone marrow compromise the usual production of normal red cells, white blood cells, and platelets that are manufactured in the bone marrow.
There are approximately 1,000 new cases of hairy cell leukemia discovered every year in the United States. There is an unexplained larger number of men than women afflicted with this leukemia. Hairy cell leukemia is treatable, but not curable. While the cause is not known, the treatment is usually very effective in helping patients lead a normal life.
Diagnosis of Hairy Cell Leukemia
Patients with hairy cell leukemia may develop many different symptoms. A physician should use careful clinical judgement to accurately diagnose a patient’s disease.
In some patients with hairy cell leukemia, the doctor can feel an enlarged spleen on physical examination. The spleen is located in the upper left side of the abdomen and when it is particularly large it may cause symptoms such as early fullness during a meal.
In early research carried out by Dr. Bertha Bouroncle, an enlarged spleen was found in more than 90% of patients with hairy cell leukemia. However, the finding of an enlarged spleen has become less common over the years due to the more frequent use of blood tests to diagnose hairy cell leukemia. Patients now will commonly have low blood counts (hemoglobin, neutrophils and monocytes) in the absence of any symptoms. Thrombocytopenia is also very common. Therefore, the failure to identify an enlarged spleen does not preclude the diagnosis of hairy cell leukemia.
To find the cause of an enlarged spleen or the reason for an abnormal blood test, more investigations will need to be done, generally by a hematologist. It may be necessary for the hematologist to order a full blood count (test that measures many features and components of the blood) and other blood tests such as a peripheral blood smear (test used to look for abnormalities in blood cells), immunophenotyping (process that uses antibodies to identify cells based on the markers on the surface of the cells), a bone marrow biopsy, and imaging tests like an ultrasound or a CAT scan of the abdomen.
The full blood count test will often show anemia (low red blood cell count that can predispose to fatigue), low white blood cell count (that can predispose to infection), and a low platelet count (that can predispose to bleeding).
The peripheral blood smear will often show a reduction or absence of a type of white blood cells called monocytes, and may document the appearance of cells with a pale cytoplasm with a “hairy” rim. These leukemic cells have a distinct appearance under the microscope. If they are not seen, this does not exclude a diagnosis of hairy cell leukemia, as the hairy cells may be found in the bone marrow only.
Immunophenotyping is a test that helps identify the hairy cells with the use of markers (so called ‘clusters of differentiation’ or CD) by ‘monoclonal antibodies’, each of which has a number or a name and will be expressed on all the malignant cells. The characteristic immunophenotype shows positivity of the leukemic cells for CD19, CD20, CD11c, CD25, CD103, CD123. Their co-expression on the hairy cells confirms the diagnostic features of “classic HCL”. There are other markers such as CD200 that are also positive.
In the variant form of HCL, the leukemic cells are negative for CD25 and CD123 and the leukemic cell count in the peripheral blood is generally high.
The absolute numbers of these leukemic cells can be useful in establishing the diagnosis and determining when treatment should be initiated.
A bone marrow biopsy is performed by using a needle to take a sample of bone near the rear area of the hip. While this can be painful, the physician can give both local and other medication to reduce the pain. This procedure is relatively quick, and provides a very useful confirmation of the diagnosis. The bone marrow biopsy consists of two separate assessments. The first assessment is called bone marrow aspirate. This test will allow the hematologist to find hairy cells in the bone marrow on a smear and by immunophenotyping like in the peripheral blood. The other test is called bone marrow trephine. This type of biopsy will be reviewed by a specialized pathologist who will look at the architecture of the bone marrow and other characteristics of the hairy cells to complete the diagnosis.
An accurate diagnosis is necessary to determine the correct treatment for each patient. It may be helpful to seek consultation at a Center of Excellence.
Symptoms of Hairy Cell Leukemia
Patients with hairy cell leukemia often have a slow onset of symptoms and may not be diagnosed for several months or even years of illness. The symptoms of hairy cell leukemia can be divided into those related to the effects due to bone marrow involvement, effects due to other organ involvement, and secondary complications due to infections or autoimmunity.
Bone Marrow Disease
Hairy cell leukemia is thought to develop in the bone marrow and as the hairy cell leukemia progresses, the normal function of the bone marrow decreases. The normal function of the bone marrow is to produce white blood cells, red blood cells (that carry hemoglobin) and platelets.
Decreased hemoglobin, which can cause anemia, can develop slowly and drop to very low levels. This can result in marked fatigue and weakness, shortness of breath, and/or dizziness.
A decrease in the white blood cells (these cells make up the immune system) can lead to recurrent infections such as pneumonia, bronchitis, etc.
The platelets can decrease to life-threatening levels, where severe spontaneous bleeding can occur. Patients may notice nosebleeds or gum bleeding, increased bruising, or even severe bleeding from their stomach.
Organ Involvement
Even though hairy cell leukemia develops in the bone marrow, it commonly travels to other organs as well. A common finding in patients is an enlarged spleen two to three times normal size. This can cause pain on the left side where the spleen is located, early feeling of fullness in the stomach, and in some cases severe pain.
The liver may also be involved, leading to pain on the right side, abnormalities of the liver function, or accumulation of fluid in the abdomen called ascites. Although uncommon, hairy cells can invade the bones and cause bone destruction with severe pain. Lymph nodes may be affected and enlargement can cause pain, whether in nodes in the neck or the abdomen. Rarely, there can be involvement in the brain causing headaches or abnormalities of brain function.
Secondary Complications
Patients with hairy cell leukemia have disturbed immune systems due to changes in their blood cells. Infections due to fungus and viruses can affect the skin, lungs, liver, or brain. Symptoms from these can include fever, cough, rashes, headaches or confusion.
Autoimmune disease may be seen in up to one-third of patients and usually causes inflammation of blood vessels or joints. Patients may have increased joint pain and swelling, unusual skin rashes, fever and/or weight loss. This can occur at the beginning or any time after diagnosis.
Summary
Patients with hairy cell leukemia may develop many different symptoms due to their illness, and patients and doctors should be aware of the many associated problems that can occur. The slow onset of the disease and its rarity may lead to the accurate diagnosis being missed or delayed. It may be helpful to consult a hairy cell leukemia expert at a Centers of Excellence.
Treatment for Hairy Cell Leukemia
Hairy Cell Leukemia (HCL) is a rare malignancy, but one of the most successfully treated of all leukemias. Since the advent of effective agents in the 1980s, most patients will enjoy very prolonged disease remission. Although current treatment is not considered curative, different therapies can be given sequentially as needed to control the disease.
Careful and experienced clinical judgment is necessary to make the most appropriate decision for each individual patient regarding the optimal time to start treatment as well as which agent to select to treat the patient’s HCL.
When to start treatment?
The decision of when to start treatment depends upon the character of the symptoms experienced by the patient and the degree of abnormality in the blood count.
Not all patients will require treatment immediately after the diagnosis is made and can be monitored until it is needed. This is termed “active monitoring” and helps avoid the potential side effects of treatment when not necessary. This watch and wait approach can be difficult and anxiety-provoking for patients and their families. However, unlike other types of cancer or some other more acute subtypes of leukemias, it is safe to wait to start treatment for hairy cell leukemia until there are more definite signs that treatment is really needed.
Many patients will clearly need treatment at the time of diagnosis because they have symptoms which may be disease-related and/or very low blood counts. A reduction in blood counts is the usual reason for initiating treatment and it is safest not to wait until the blood counts fall to very low levels, even if the patient feels relatively well.
Three types of cells may be reduced – red blood cells (low red blood cell counts cause anemia and symptoms like tiredness and loss of energy), white blood cells (which are needed to help fight infection), and platelets (which prevent abnormal bleeding and bruising). Not all of the above cell types may be low at the same time. However, patients with HCL most commonly have a reduced ability to fight infection and so treatment of the hairy cells is needed to help restore this capability.
The major drugs used to treat HCL can temporarily lower the blood counts before they eventually improve, so careful attention and efforts to control active infection are needed. It is important to always treat any active infection effectively before starting initial or continuing therapy for the HCL itself.
After treatment there is almost always a further, temporary fall in normal blood counts before they eventually recover. This is because it takes time for the disease to clear from the bone marrow. Recovery usually takes 3-6 weeks, but it depends on the treatment and the patient’s response.
Which treatment to use?
For the past 30 years, the mainstay of treatment for HCL has been pentostatin and cladribine, two drugs in the class called purine analogues. Pentostatin was introduced in the 1980s followed by cladribine in the early 1990s. Today, there is a great deal of experience and long-term follow up using these two agents. Both are highly effective in inducing clinical response and a remission (in almost all patients), with no significant difference in efficacy between the two. Most of these remissions are complete (i.e., no evidence of any remaining disease in the bone marrow using standard methods). Such remissions often last for prolonged periods of time, sometimes even more than 10 years.
In September 2018, moxetumomab pasudotox, an anti-CD22 immunotoxin, was approved by the U.S. Food and Drug Administration (FDA) for the treatment of adult patients with HCL who have already received at least two prior systemic therapies, including treatment with a purine nucleoside analog. Approval was based on a clinical study of 80 patients with HCL or HCL variant: 77 with classic HCL and 3 with HCL variant. Of these patients, 41% achieved complete remission (CR). Most CRs were without minimal residual disease, which if still present may eventually result in relapse. The approval of moxetumomab pasudotox by the FDA represents an exciting new treatment for patients whose leukemia develop resistance to standard treatments.
How are drugs used to treat hairy cell leukemia currently administered? What are the usual side effects?
Pentostatin is administered as a short intravenous (IV) infusion every 2-3 weeks until a remission is achieved. Pentostatin is excreted from the body by the kidneys and thus it is important to check kidney function to ensure that it is normal before giving the drug. Patients can experience nausea up to 72 hours after the infusion and they should have anti-nausea medication available in case they need it.
Cladribine can be given in a number of ways, including as a 7- day continuous IV infusion (which may require hospital admission), daily IV infusion over 2 hours for 5 doses or weekly for 6 doses, or as a subcutaneous injection on 5 consecutive days. All modes of administration have been shown to be effective. The choice will largely depend on the physician and patient and most are given as outpatient treatment.
Both drugs are generally well tolerated but are associated with a temporary reduction in normal blood counts, which need to be monitored closely (weekly initially) until recovery. Sometimes recovery of the reduced blood counts is delayed for a much longer time, but eventually they improve.
Pentostatin and cladribine may also cause a more prolonged suppression of the immune system, and patients should be informed of this possibility and be made aware of signs and symptoms of possible infection. Infections should always be taken seriously as prompt treatment is important. Some doctors will also administer low doses of antibiotic/antiviral agents in order to reduce the risk of infection. In the case of cladribine, it is better to start these agents after the 1-week course of treatment has been given, since rashes can sometimes occur when the drugs are given concurrently. Blood transfusions, if ever required, should be with irradiated blood.
Splenectomy is rarely performed nowadays since the agents used today are very effective in reducing the size of the spleen. The spleen is often enlarged at the time of diagnosis.
Interferon was used in the past, but is rarely used today. It is not well tolerated and much less effective than the purine analogues, but occasionally may still be useful if patients fail initial therapy.
Rituximab used as a single agent in first line treatment of HCL is not as effective in inducing remissions as the purine analogues. Its use would be reserved for patients unable to tolerate purine analogues. There is evidence that better remissions may be achieved with the combination of rituximab and a purine analogue (pentostatin or cladribine). Because of the very good results with purine analogues alone for most patients, the addition of rituximab is often reserved for those HCL patients who do not achieve a complete remission or who relapse earlier than expected.
Targeted therapies such as BRAF inhibitors (vemurafenib) and B-cell receptor inhibitors (ibrutinib) have activity in HCL. Currently, these therapies have been examined in relapsed or refractory HCL and only in a very small number of patients for whom purine analogues cannot be given as first line therapy. A number of clinical trials are ongoing to evaluate these drugs further in hopes of sparing the immunosuppressive effects of purine analogues.
Moxetumumab pasudotox (Lumoxiti) is administered as an intravenous infusion over 30 minutes on days 1, 3, and 5 of each 28-day cycle. Lumoxiti may cause serious side effects, including capillary leak syndrome and hemolytic uremic syndrome.
HCL is a rare disease and there are very few clinical studies being undertaken worldwide. To continue to make progress in new therapies, it is important for patients at every stage of treatment to consider participation in clinical trials. We encourage patients to visit our clinical trials page to learn about trials underway that may be right for them.
Assessment of Response and Monitoring
Usually within a few weeks of receiving treatment, the blood counts begin to recover and will often return to completely normal levels. However, to assess response to anti-HCL treatment, a bone marrow examination is necessary. This is usually done 3-4 months after cladribine therapy to assess the full impact of therapy. The bone marrow procedure is not pleasant for patients, but does provide important information about the quality of response to the treatment given and whether or not more or different therapy is needed. Studies have shown that in those patients who have obtained a clinical complete remission, the response lasts longer. There are other more sensitive laboratory methods which can assess for any measurable minimal residual disease (MRD). MRD may be present even if patients are in complete remission. It remains to be determined what effect the presence of MRD has on outcome and this is an area of ongoing research.
About 40% of patients will relapse, even 10 years or more after initial therapy. Regular monitoring by a hematologist takes place, usually once or twice a year for patients in stable remission. Relapse is usually suspected in patients who have falling blood counts and should be confirmed by examination of the bone marrow. Re-treatment is often successful although the subsequent remissions tend to last for a shorter period of time, when the same therapeutic agents are given again.
Complications of Hairy Cell Leukemia
Hairy cell leukemia most commonly affects the bone marrow and spleen. However, because HCL travels between the bone marrow, spleen, liver and lymph nodes via the bloodstream, it may potentially affect any part of the body that the blood circulates to. Therefore, other medical problems have been described that are likely a direct or indirect result of the hairy cell leukemia. This section will provide a brief review of both the common and uncommon complications of HCL.
When hairy cell leukemia is present in the bone marrow, it slowly increases over time until it begins to prevent normal blood cell production. This leads to lowering of the normal blood counts and may be manifested as low red cell counts (anemia), low platelet counts (thrombocytopenia), and/or lower than normal white blood cells (neutropenia, lymphocytopenia, and monocytopenia). Many of the symptoms and complications of HCL are a direct result of low blood cell counts.
In some patients, hairy cells will begin to circulate in the blood stream and when this happens the white blood count may be higher than normal. Some patients with hairy cell leukemia have an elevated white blood cell count due to the presence of hairy cells in the bloodstream, but these are not normally functioning white blood cells and do not protect against infection. Whether the white blood count is high or low, patients with HCL are overall at increased risk of infection. In fact, infection is one of the leading causes of illness and death for patients with hairy cell leukemia. Infections can be caused by bacteria, viruses, or fungal diseases. In addition, some medications used to treat HCL can temporarily increase the risk of infection by decreasing the white blood cell numbers or normal functioning. For example, the chemotherapy agents most commonly used for the initial treatment of hairy cell leukemia - pentostatin and cladribine - can lower the number of normal lymphocytes. This side effect of therapy can last for many months and increase the patient’s risk of developing a viral disease (e.g., Herpes Zoster, commonly called shingles) or fungal disease that can cause pneumonia. Patients with HCL should not receive the older Herpes Zoster (shingles) vaccine (called Zostavax) from their physicians, as it is a live virus vaccine that might result in causing the very condition that it is intended to prevent. However, immunizations using killed virus vaccines, such as the influenza vaccine, are safe and may provide important protection for HCL patients. A newer, non-live shingles vaccine (called Shingrix) has more recently been introduced and patients with HCL should discuss this option with their doctors.
Lowering of the red blood cell count, or anemia, is often associated with symptoms of fatigue. Some patients with hairy cell leukemia will require a red blood cell transfusion to correct this problem, although this is a temporary solution until the HCL improves. Lowering of the platelet counts leads to an increased tendency to bleed, and many patients with low platelet counts notice an increased tendency to develop bruising or bleeding from the gums or nose. If bleeding is severe or the platelet count is very low, a platelet transfusion may be required. However, again this is a temporary solution until treatment is given to improve the underlying HCL.
In the past, significant enlargement of the spleen was a very common complication of hairy cell leukemia and was often the initial symptom of the disease. Although patients today are more often diagnosed with HCL on the basis of an abnormal blood count, many patients will still develop an enlarged spleen as part of the disease course. This may cause symptoms of abdominal pain, abdominal distention, or difficulty eating a full meal due to the pressure that the enlarged spleen exerts on the stomach. Most of the effective therapies for HCL will decrease the size of the spleen, relieving these discomforts.
It is possible to remove the spleen if need be, although this could lead to an increased risk of certain types of infection. Therefore, removing the spleen is usually only performed if other therapies are not possible or have not proven effective. When the spleen is very enlarged there is an increased risk of splenic rupture due to trauma, such as a car accident. Sudden pain in the abdomen followed by profound weakness should cause the patient to seek immediate medical care in an emergency facility.
There has been some concern that the therapy for hairy cell leukemia may increase the patient’s risk for developing a secondary cancer. This is an ongoing issue of debate. Some studies show that the disease itself may actually increase this risk. Therefore, people with HCL should continue to have their routine cancer screening performed at regular intervals based upon recommendations established by cancer experts.
Further defining the more rare complications of hairy cell leukemia is an ongoing research initiative. For example, there is some suggestion that certain types of autoimmune complications many manifest in patients with HCL, such as certain types of arthritis and immune-mediated blood disorders. Understanding the complications of hairy cell leukemia is one of the main goals of the HCL Patient Data Registry, and the valuable insights gained by this project will add to the understanding of this rare disease.
Refractory or Resistant Disease: When Patients with Hairy Cell Leukemia Don’t Respond to Treatment
Confirming the correct diagnosis of hairy cell leukemia: For those patients with hairy cell leukemia who don’t respond to front-line drugs (cladribine or pentostatin), it is important to establish that the correct diagnosis was made. This normally requires flow cytometry of the blood (laser-based technology that analyzes characteristics of cells) and preferably of the bone marrow. There are specific markers that are characteristically found on the leukemic cells from patients with classic hairy cell leukemia. The markers on the leukemic cells may provide a clue that the non-responding patient has a variant of hairy cell leukemia. These patients can undergo analysis of the BRAF expression to further delineate whether the patient has either the classic form of the disease or a variant. Confirmation of the underlying diagnosis enables decisions to be made about treatment.
Patients with the atypical variant of hairy cell leukemia do not respond as well to the standard agents and may have a short-lived, partial response. The variant form of hairy cell leukemia is now recognized as a separate clinical entity from the classic disease, and is recognized as being less responsive to therapy with standard treatment. Some patients with the variant form of hairy cell leukemia have responded to the combination of cladribine and rituximab. In addition, moxetumomab pasudotox was more recently approved by the FDA for the treatment of adult patients with hairy cell leukemia and hairy cell leukemia variant who have received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
Confirming why the patient is not responding: For patients with hairy cell leukemia who do not seem to respond to treatment (often called “assumed failure to respond”), it is important to accurately confirm the response before the patient undergoes re-treatment. For example, in some cases, patients have low blood counts for months after treatment, due to the toxicity of either cladribine or pentostatin. Given time, the patients in these cases may achieve a remission. Furthermore, some patients may develop “resistant” disease after having had multiple relapses with progressively shorter remission durations over time. It is important to understand why the patient is not responding to treatment (i.e., either incorrect diagnosis, delayed recovery from treatment-induced toxicity, or eventual evolution of resistant clones of leukemic cells following extensive prior treatments). If the patient is non-responsive to medical therapy, splenectomy may be required.
Evaluation of the patient by a hematologist with experience in the management of hairy cell leukemia may enable the reason for the patient’s lack of response to be understood. To avoid being retreated too early or unnecessarily, it may be helpful to consult an HCL expert at a Centers of Excellence.
Understanding Relapse of Hairy Cell Leukemia
Patients who are treated for hairy cell leukemia should have a bone marrow biopsy performed following treatment to determine if a complete response (eradication of all evidence of hairy cell leukemia) has been achieved. Among patients who have achieved a complete response, it is not unusual to find minimal residual disease (MRD) if more sophisticated studies are done to detect a small amount of hairy cells not visible under the regular microscope. Minimal residual disease may be one reason that some patients ultimately relapse.
Patients are usually followed quarterly after they have completed therapy. Routine blood counts are obtained to ensure that the remission is being maintained. If blood counts show a decline, a repeat bone marrow may be obtained to see if the disease is relapsing by identifying a small amount of recurrent hairy cells. Immunophenotyping studies (looking for certain markers on the surface of the lymphocytes to identify hairy cells) may be done to look for a small amount of recurrent hairy cells.
If relapse has been documented, careful consideration is given to decide if and when to re-initiate treatment. Just as there is a watchful waiting approach at the time of initial diagnosis, a similar strategy may be followed in patients who have a small amount of recurrent hairy cells, but are without symptoms. A small decline in the blood counts may not be sufficient to warrant re-treatment since often this disease is slow-growing. However, there is an advantage to re-starting therapy before the counts deteriorate to very low dangerous levels.
Hairy Cell Leukemia variant
What is HCL variant?
Hairy cell leukemia variant (HCL-V) is an unclassifiable splenic B-cell leukemia/lymphoma. According to the World Health Organization classification of diseases, it is not biologically related to classic hairy cell leukemia. HCL-V is a more aggressive disease than the classic form.
Epidemiology
Hairy cell leukemia variant is a rare disorder accounting for approximately 0.4% of chronic lymphoid malignancies and 10% of all HCL cases. The disease affects the elderly population without sexual predominance. The median age of the patients is 71 years.
Diagnosis
A diagnosis of hairy cell leukemia variant should be established by morphological analysis (referring to the structure and shape of cells) and flow cytometric analysis (referring to a method of measuring certain characteristics of cells) of peripheral blood, bone marrow and/or spleen specimens. The features of hairy cell leukemia variant are intermediate between those of classical HCL and prolymphocytic leukemia (PLL).
Patients with HCL-V have elevated white blood cells as well as unique morphology (structure and shape) and immunophenotype (types of markers on the surface of cells). HCL-V cells are CD19+, CD20+ and CD22+, and are positive for B-cell antigens on flow cytometric analysis. Leukemic cells are also positive for CD103 and CD11c and negative for CD25. In contrast to the classic hairy cell leukemia, patients with HCL-V have no monocytopenia (deficiency of monocytes, a type of immune cell that is made in the bone marrow), and the leukemic leukocytes lack CD25 antigens. Moreover, HCL-V is not associated with the BRAF V600E mutation.
Treatment
There is currently no curative treatment for hairy cell leukemia variant. The results of therapy with cladribine or pentostatin are rather poor. An analysis of 19 cases reported in various treatment centers showed a response rate of 55%, including only two complete remissions. In addition, the majority of HCL-V patients required more than one cycle to maintain a partial remission. Pentostatin induced a partial remission in 8 out of 15 (54%) patients, but no complete remission was observed.
Rituximab alone or splenectomy followed by rituximab therapy can induce complete remission in patients with hairy cell leukemia variant. More recently, cladribine combined with rituximab was found to be more effective than cladribine alone or rituximab alone. Kreitman et al report a case of 10 patients with HCL-V treated simultaneously with cladribine and rituximab. Nine patients (90%) achieved a complete remission with this regimen, compared with 3 of 39 cases (8%) reported in the literature who were treated with cladribine alone. In addition, 7 patients (88%) had a complete remission with minimal residual disease negativity at 12-38 months of follow-up. These results indicate that patients with HCL-V could be initially treated with cladribine combined with rituximab.
Alemtuzumab is an active agent in selected cases with hairy cell leukemia variant. Splenectomy can induce clinical responses and correct cytopenias (lower-than-normal number of blood cells) in some patients with HCL-V. In one study, splenectomy resulted in good partial remission in 2/3 patients. Some case studies indicate that autologous transplantation (blood-forming stem cells are removed, stored, and later given back to the same person) or allogenic hematopoietic cell transplantation (a person receives blood-forming stem cells from a genetically similar, but not identical, donor) can be effective in patients who don’t respond to other treatments.
Moxetumomab pasudotox, an anti-CD22 immunotoxin, was more recently approved by the U.S. Food and Drug Administration (FDA) for the treatment of adult patients with hairy cell leukemia or hairy cell leukemia variant who received at least two prior systemic therapies, including treatment with a purine nucleoside analog. Approval was based on a clinical study of 80 patients with HCL or HCL variant: 77 with classic HCL and 3 with HCL variant. 41% of patients experienced complete remission (CR) and most CRs were without minimal residual disease, which may cause relapse.
Emerging Drugs
The B-cell antigen receptor (BCR) signal transduction inhibitors, ibrutinib (PCI-32765) and idelalisib (GS-1101, CAL-101), represent a promising new strategy for the treatment of hairy cell leukemia and possibly hairy cell leukemia variant.
History of Hairy Cell Leukemia
In 1958, Dr. Bouroncle described the multiple features of hairy cell leukemia, firmly establishing this disease as a unique clinical entity. The malignant cells were identified predominantly in the bone marrow, spleen and other tissues. The morphologic description (referring to the form and structure) of this malignant cell was so unique that it was subsequently called “hairy cell leukemia” consistent with the serrated border of the cytoplasm. While the origin of this malignant cell was often debated, it has ultimately been recognized as a B-cell malignancy with a very distinctive immunophenotypic profile.
For the latter part of the past century, the diagnosis was made by describing these leukemic cells in the peripheral blood and the bone marrow. Classic hairy cell leukemia has been differentiated from the less common variant form of this leukemia, which is now known to be a completely separate clinical entity. The leukemic presentation of the variant form of this disease may be associated with bone marrow failure and significant splenomegaly, but the diagnostic markers differ from the classic form of the disease as does the clinical course and response to therapy.
In 2011, Dr. Tiacci and colleagues described the presence of BRAFV600E mutation in leukemic cells from almost every patient with the classic form of hairy cell leukemia. In sharp contrast, this mutation is missing in the variant form of the disease. This observation has provided diagnostic accuracy as well as a novel therapeutic target for patients with the classic form of the disease. In patients who have been unresponsive to standard effective therapy for classic hairy cell leukemia, clinical responses have been observed in patients treated with BRAFV600E inhibitors. Both vemurafenib and dabrafenib have been reported to induce remissions in patients with relapsed or refractory disease.
In the 1950’s, Bouroncle and colleagues reported that the classic form of hairy cell leukemia had a variable chronic course, and the overall survival was in the range of 4 to 6 years. The patient bone marrow was routinely very fibrotic and involved with the leukemic cells, making tolerance to standard cytotoxic agents very challenging. Consequently, splenectomy became the therapy of choice to correct the “cytopenias” that frequently complicated the clinical course for these patients. While splenectomy improved the blood counts, the response was usually limited.
In 1984, Quesda and colleagues reported the remarkable results with daily alpha interferon. Despite symptoms related to the use of this biologic agent (e.g., fatigue and influenza-like symptoms), the improvement in hematologic parameters was dramatic. Granulocyte numbers improved both in the bone marrow and the peripheral blood. Splenomegaly gradually improved as the blood counts responded over several months. While more than 80% of patients achieved a response to alpha interferon, less than 20% achieved a complete remission. Furthermore, responses were in general short-lived. In the same period, a report by Spiers showed that pentostatin was capable of inducing a complete remission in a limited number of patients with hairy cell leukemia. Shortly thereafter, other investigators showed that durable complete remissions could be achieved with lower doses of pentostatin. In a large randomized trial, Grever showed that pentostatin produced complete remission in more than 75% of patients and was markedly more effective than alpha-interferon.
In 1990, Piro and colleagues showed that very promising responses could also be achieved with a seven-day intravenous infusion with cladribine. These responses were sustained. While the complete remission rate was reported to be greater than 90%, the rate of febrile neutropenia was higher with cladribine compared to pentostatin. This raised the possibility that pentostatin might be less likely to induce treatment-related infection. Both agents have now been confirmed as highly effective front-line therapy for newly diagnosed patients with hairy cell leukemia.
Despite the success and the impact of using either purine nucleoside analog, some patients will either relapse or be unresponsive to the initial induction therapy.
Moxetumomab pasudotox (LUMOXITI), an anti-CD22 immunotoxin, was approved by the U.S. Food and Drug Administration (FDA) in September 2018 for the treatment of adult patients with hairy cell leukemia who received at least two prior systemic therapies, including treatment with a purine nucleoside analog.
Exploration and further evaluation of alternative therapy options will continue to be important to achieve durable complete remission for all patients with hairy cell leukemia.